Effects of somatropin on the body
Pharmacological properties
Pharmacodynamics
Stimulates skeletal and somatic growth and has a pronounced effect on metabolic processes.
Stimulates skeletal bone growth by acting on the epiphysis plates of tubular bones, bone metabolism in children.
Promotes normalisation of body structure by increasing muscle mass and reducing body fat.
In patients with growth hormone (GH) deficiency and osteoporosis, replacement therapy leads to normalisation of bone mineral composition and density.
Increases the number and size of cells in muscle, liver, thymus gland, sex glands, adrenal glands, thyroid gland.
Stimulates amino acid transport into the cell and protein synthesis, reduces cholesterol concentration by affecting lipid and lipoprotein profile.
Suppresses the release of insulin. Promotes sodium, potassium and phosphorus retention.
Increases body weight, muscular activity and physical endurance.
Pharmacokinetics
Absorption of somatropin after subcutaneous administration is 80%, maximum plasma concentration is reached in 3-6 hours.
It penetrates into well perfused organs, especially liver and kidneys.
The volume of distribution of somatropin is 0.49 – 2.11 l/kg.
The half-life after subcutaneous administration is 3-5 hours.
Indications for use
Growth retardation in children due to insufficient secretion of GH, in Shereshevsky-Turner syndrome, in chronic renal failure (decrease in renal function by more than 50%) in prepubertal period.
In adults with confirmed severe congenital or acquired GH deficiency as replacement therapy.
Contraindications
Hypersensitivity, malignant neoplasms, urgent conditions (including conditions after heart surgery, abdominal cavity, acute respiratory failure). Stimulation of growth in patients with closed epiphyseal growth zones.
Pregnancy and breastfeeding (breastfeeding should be avoided for the duration of treatment).
With caution: diabetes mellitus, intracranial hypertension, hypothyroidism, concomitant therapy with glucocorticosteroids, hypothyroidism (including during thyroid hormone replacement therapy), Prader-Willi syndrome.
Method of administration and dosage
The drug is administered subcutaneously, slowly, once a day, usually at night. It is necessary to change injection sites to prevent the development of lipoatrophy.
Doses are selected individually taking into account the severity of GH deficiency, body weight or surface area, effectiveness in the course of therapy.
In children with insufficient GH secretion a dose of 25-35 µg/kg/day (0.07 – 0.1 IU/kg/day) is recommended, which corresponds to 0.7 – 1 mg/m 2 /day (2 – 3 IU/m²/day). Treatment should be started as early as possible and continued until puberty and/or until the bone growth zones are closed. Treatment may be discontinued when the desired result is achieved.
A dose of 45 – 50 µg/kg/day (0.14 IU/kg/day), corresponding to 1.4 mg/m 2 /day (4.3 IU/m²/day), is recommended in Sherechevsky-Turner syndrome, in chronic renal failure in children with growth retardation.
Dose adjustment may be necessary in case of insufficient growth dynamics.
In GH deficiency in adults, the initial dose is 0.15-0.3 mg/day (corresponding to 0.45 – 0.9 IU/day) with its subsequent increase, depending on the effect.
When titrating the dose, serum insulin-like growth factor (IGF-I) concentration can be used as a control indicator. The maintenance dose is selected individually, but does not exceed, as a rule, 1 mg/day, which corresponds to 3 IU/day.
Lower doses are recommended for the elderly.
Side effects
Increased intracranial pressure (headache, nausea, vomiting, visual disturbance), decreased thyroid function, hyperglycaemia, leukaemoid reactions, epiphyseolysis of the femoral head, fluid retention with the development of peripheral oedema. Symptoms are usually transient, dose-dependent, may require dose reduction. Allergic reactions: skin rash, itching. Local reactions: soreness, numbness, hyperaemia, swelling, lipoatrophy at the injection site.
Warning. The following side effects have been described in the literature when using somatropin: weakness, fatigue, gynaecomastia, optic disc oedema (usually seen during the first 8 weeks of treatment, most common in patients with Shereshevsky-Turner syndrome), pancreatitis (abdominal pain, nausea, vomiting), otitis media and hearing impairment (in patients with Shereshevsky-Turner syndrome), hip subluxation in children (limp, pain in the hip and knee), gynaecomastia, acceleration of growth of pre-existing nevus (possible malignisation), progression of scoliosis (in patients with excessively rapid growth), increase in blood inorganic phosphate, parathyroid hormone and alkaline phosphatase activity.
Overdose
Acute overdose may lead initially to hypoglycaemia and then to hyperglycaemia. In case of prolonged overdose, signs and symptoms characteristic of human GH excess – development of acromegaly and/or gigantism, as well as development of hypothyroidism, decrease in serum cortisol concentration may be observed. Treatment: cancellation of the drug, symptomatic therapy.
Interaction with other medicinal products
Somatropin increases clearance of drugs metabolised by liver microsomal enzymes, especially sex hormones, glucocorticosteroids, anticonvulsants and cyclosporine. Glucocorticosteroids inhibit the stimulating effect of somatropin on growth processes. Concomitant therapy with other hormones, e.g. gonadotropin, anabolic steroids, estrogens and thyroid hormones, may also influence the efficacy of the drug (in terms of final growth).
Special instructions
Against the background of Rastan treatment it may be necessary to correct doses of hypoglycemic drugs in patients with diabetes mellitus, latent hypothyroidism may manifest, and in patients receiving levothyroxine sodium, signs of hyperthyroidism may appear. During treatment it is necessary to monitor the state of the ocular fundus, especially in case of symptoms of intracranial hypertension. Optic disc edema requires cancellation of the drug. Detection of claudication against the background of somatropin therapy requires careful monitoring. It is necessary to change the sites of subcutaneous injections due to the possibility of lipoatrophy development. During kidney transplantation treatment with the drug should be cancelled. Provided that there are no symptoms of increased intracranial pressure (headache, nausea, vomiting, visual disturbance), somatropin does not affect the ability to drive vehicles and engage in other potentially dangerous activities requiring increased concentration and rapid psychomotor reactions.
Showing 1–16 of 29 results
-
ATECHTROPIN – HGH 3,7 mg A-Tech Labs
395,00 € Add to cart -

Deustropin Somatropin HGH 120 IU Deus Medical
370,00 € Add to cart -

Eurotropin 40 IU Euro Pharmacies
144,00 € Add to cart -
Evogene 100 IU Alley
170,00 € Add to cart -

G-TROPIN (Somatropinum) 100 IU Euro Pharmacies
289,00 € Add to cart -

Genotropin 12mg/ml GoQuick
755,00 € Add to cart -

GENOTROPIN MiniQuick 0.2mg Pfizer
88,30 € Add to cart -

Genotropin Pen 12 mg 36 IU Pfizer
360,00 € Add to cart -
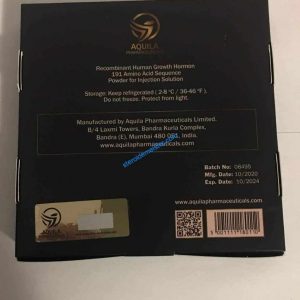
HGH (Somatropin) 100 IU Aquila Pharmaceuticals
450,00 € Add to cart -

HGH Blue Top 100 IU Pharmazeutik
166,00 € Add to cart -

HGH Somatropin 15 IU 5 mg Pharm Chemical
94,50 € Add to cart -

Humalog 100 IU – KwikPen – 5 x 3 ml Fertigpens – Eli Lilly
55,00 € Add to cart -

Humalog 100 IU – KwikPen – 5 x 3 ml Patronen – Eli Lilly
65,00 € Add to cart -

Humatrop (Somatropin) – 18 IU(6 mg) – Eli Lilly
182,00 € Add to cart -

Humatrope 12 mg 36 IU Lilly
350,00 € Add to cart -

Humatrope 72 IU Lilly
280,00 € Add to cart
